-
How Can You Prevent Depression?

A patient who had completed traditional Chinese medicine for acne told me, “Doctor, Chinese medicine is incredible! I used to be easily irritated, but after taking your traditional Chinese medicine, I didn’t even get angry when someone stepped on my white sneakers. My personality has changed…haha~”
The doctor responded, saying: “In fact, traditional Chinese medicine has been used to treat mood disorders since ancient times. Mood disorders, according to traditional Chinese medicine, are caused by an imbalance of yin and yang and a lack of smooth qi. The mood can be effectively improved as long as the yin and yang deviation and the qi mechanism are well adjusted.”
The Yellow Emperor’s Classic of Medicine state that
“Excess of joy affects the heart
Excess of anger affects the liver
Excess of thinking affects the spleen
Excess of sadness affects the lungs
Excess of fear affects the kidneys”Emotions, in fact, are neither good nor bad; they are the natural expression of human beings. However, if an emotion is “too much” or “not enough,” it can have a negative impact on health. As a result, we should prioritise our emotional health. If we discover that our emotions are slightly skewed, we can begin with traditional Chinese medicine or acupuncture. Traditional Chinese medicine treatment typically employs natural Chinese herbal medicine, which has fewer side effects and does not lead to drug dependence.
For example, “逍遙散Xiaoyao San” and “甘麥大棗湯Ganmai Dazao Soup” are both popular formulas for emotional reconciliation. Of course, Chinese medicine places a premium on syndrome identification and treatment.
Even though the emotions have the greatest impact on health when they are excessive, some people can become ill due to a lack of emotions. Feelings and emotional stability are essential components of good mental health. Emotions that are too strong or too weak can cause physical and mental disorders. Excessive happiness, for example, can lead to mania, whereas a lack of joy can lead to psychosomatic disorders. Excessive anger can cause cardiovascular disease, insomnia , whereas a lack of anger results in a lack of motivation in life.
Depression in the elderly is a serious issue that is linked to cognitive function. What is the best way for a Chinese medicine doctor to improve mental health ?
Doctors and patients collaborate to achieve emotional balance, not too much, make balance , as this is the best way to avoid depression. -
Forward Head Posture
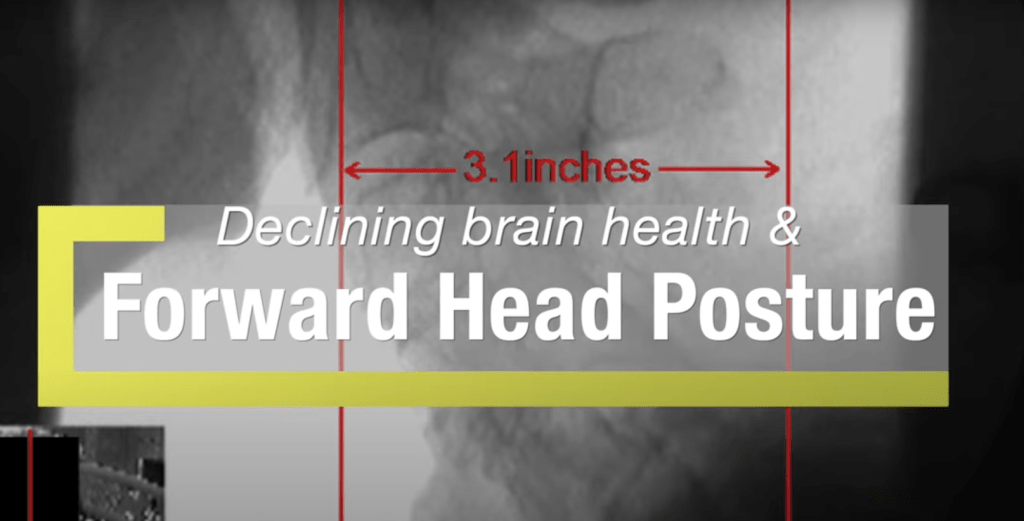
All of us watching on a cell phone for longtime a day , consequence in high pressure on our neck and shoulder muscles ,and eventually may get a forward head posture .
So , Is forward head posture a cause of dementia ?
In this video , Dr. Hauser discusses the importance of correcting forward head posture before it’s too late and leads to brain atrophy. We hope that you will put some positive changes into action in your own life to help your neck curve and brain health.
“The arterial supply needs to go up so that’s one problem then the brain can’t drain well all this cellular waste it can’t get out of the brain so what’s going to happen the pressure inside the brain is going to go up and the pressure eventually causes the neuron cells to die when the neuron cells to die .We call that brain degeneration or brain atrophy and long term that does what your memory starts going and eventually a person can get diagnosed with alzheimer’s .I ‘m not saying all alzheimer’s diseases from this.”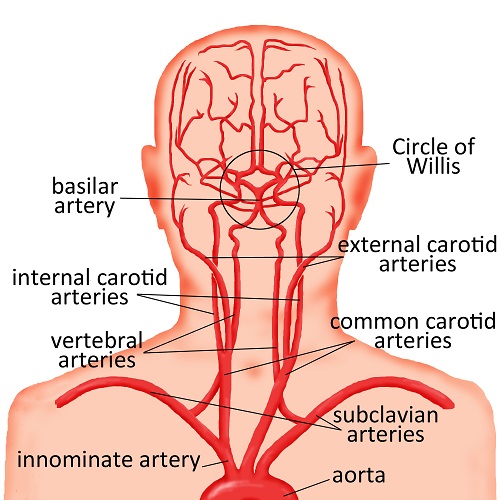
Soure from childrenswi.org What is blocked in the neck meridian
In Chinese Medicine theory , Qi ,the viral energy in the neck meridian are blocked when there is muscle imbalance occurs at the neck in a long term abnormal postition.

In this meridian chart , we can see two yellow line , which is DU meridian 督脈 and GB meridian 膽經 , and the black line , called UB meridian 膀胱經 pass through from the neck to the brain .
All this meridian bring Qi from different organs ,containing many nutrients supply to the brain to maintain daily usage of the brain activity.
In the nutshell, not just blood supply is impacted , the Qi movement and supply is blocked from forehead posture .This is the reason why as a Chinese medicine doctor , my treatment to dementia or any brain damage patients emphasis on the neck area.
There are many acupoint on that three meridians mentioned above that is so important ,like 風府穴 DU16 , and 風池穴 GB20.
We will discuss this topic in the next article .

DU 16 and GB20 -
Can TCM pass through Blood brain barrier

Blood brain barrier
The brain is a very important organ of the human body and naturally requires special protection. The blood vessels in the brain are covered with a blood-brain barrier (BBB), which helps the brain isolate the infestation of bacteria, viruses and toxic substances in the blood. Except for oxygen, sugar and a small amount of nutrients that the brain needs to pass freely, most of the substances will be isolated outside the barrier, including various proteins and macromolecules.
However, while the blood-brain barrier blocks harmful substances, it also blocks the therapeutic drugs. Whether it is traditional Chinese medicine or Western medicine, most drugs cannot enter the brain, which is naturally not a good thing for patients with brain diseases such as Alzheimer’s disease and Parkinson’s disease.
How to find a drug that can effectively pass through the blood-brain barrier becomes the key to choosing a treatment prescription. In this article, we will introduce Chinese herbal medicines that are commonly used in Chinese medicine and can cross the blood-brain barrier, so as to help you better understand the treatment options of Chinese medicine for brain diseases.

Research Name :
Studies of blood-brain barrier permeability of gastrodigenin in vitro and in vivoAccording to the basic theories of traditional Chinese medicine, Gastrodia elata (GE) is clinically utilized for the treatment of cephalalgia and migraine.

天麻
Gastrodia Elata Tian-MaThe gastrodigenin (p-hydroxybenzyl alcohol, HBA), one of the effective components of GE, may pass through the blood-brain barrier (BBB) to exert its pharmacological effects. This study aimed to investigate BBB permeability of HBA via in vitro hCMEC/D3 BBB model and in vivo microdialysis in rats. For the establishment of in vitro BBB model, hCMEC/D3 cells were used to construct the monolayer. The integrity of the monolayer was evaluated by TEER measurements, expression analysis of tight junction proteins (claudin-5, zo-1 and occludin) and apparent permeability coefficients (Papp) of fluorescein disodium. During the 6-day incubation of hCMEC/D3 cells, the values of TEER gradually increased and maintained above 100 Ω·cm2. Besides, the expression levels of claudin-5 and zo-1 in hCMEC/D3 cells increased over time, and tended to be stable, suggesting that integrity of the monolayer has been completely established. Moreover, the Papp of fluorescein disodium was 3.94 × 10-7 cm·s-1 after administration for 180 min, indicating that the monolayer retains the characteristics of BBB and can restrict the diffusion of hydrophilic small-molecule compounds. A sensitive HPLC method was established for HBA detection, and the transport rate of HBA was assessed by a transwell system. HBA crossed the hCMEC/D3 BBB model rapidly, but a plateau was observed when HBA concentrations were relatively similar between the two sides of transwell. Permeability assay revealed that 32.91% of HBA could penetrate the in vitro BBB model after 240 min of administration. In vivo BBB permeability was evaluated by determining the concentrations of HBA in blood and brain simultaneously. Following HBA administration, the samples of microdialysis were collected at 20, 40 and 60 min, and then every 30 min until the procedure ended. Pharmacokinetic parameters of HBA showed that HBA could pass through BBB and reach its maximum concentration at 40 min in blood and brain tissue. Furthermore, AUC0-t and AUC0-inf for the brain-to-blood distribution ratio of HBA were 0.1925 and 0.2083, respectively, indicating that approximately 20% of HBA in blood could pass through the BBB and subsequently transported into the brain. Both in vitro and in vivo experiments confirmed that HBA could penetrate the BBB. In summary, the findings of this study highlight that a promising amount of HBA in blood can pass through the BBB and exerts its pharmacological effects on central nervous system (CNS) diseases.
Keywords: Blood–brain barrier; Gastrodia elata; Gastrodigenin; Microdialysis; hCMEC/D3.
Reference:
Yahui Mi, Yukang Mao, Huan Cheng, Guohan Ke, Mingping Liu, Chunping Fang, Qian Wang. Studies of blood-brain barrier permeability of gastrodigenin in vitro and in vivo. Fitoterapia. 2020 Jan;140:104447. doi: 10.1016/j.fitote.2019.104447. Epub 2019 Dec 2.
http://shunkulin.blogspot.com/2021/01/blog-post_29.html
-
ChiLoveSoup -The special prescription for dementia
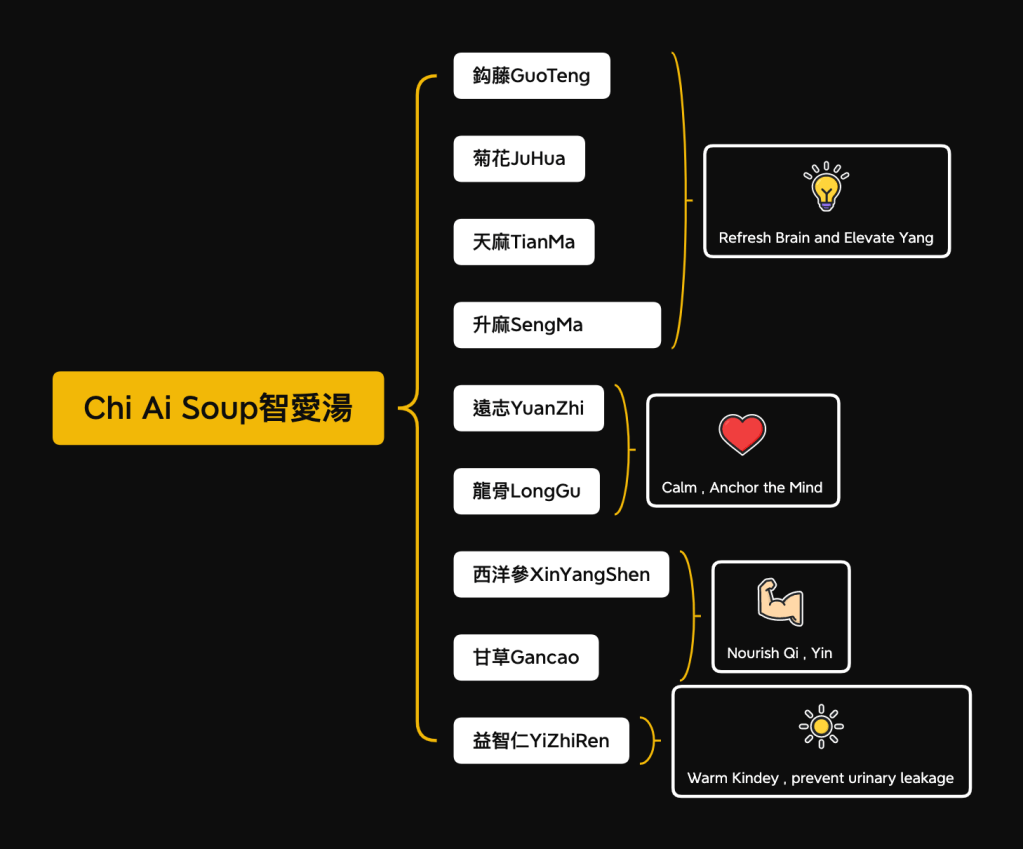
The formula established by Dr Shun-Ku Lin, MD, has found it works well in clinical studies.
Zhi Ai Decoction is a special prescription for dementia. Clinical studies have found that regular consumption of this herbal formula can slow down mental deterioration, maintain life ability, and reduce the severity of abnormal behaviors.
The main ingredients of Chi-Love-Soup are
西洋參XinYangSeng, which nourishes qi and yin,
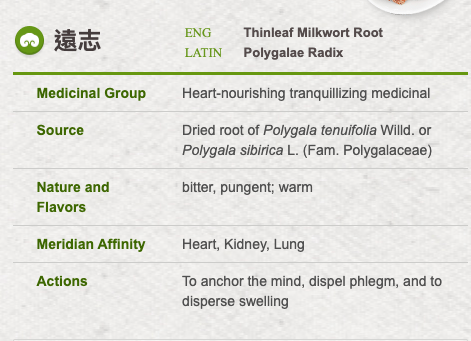
遠志Yuan zhi, which refreshes the brain,
升麻Sheng Ma , which elevate yang Qi .
Some delusions, anxiety, irritability, emotional tension and other symptoms, add 天麻Tianma, 龍骨LongGu, 鉤藤GouTeng and other soothing and shocking drugs to reduce the frequency of seizures,
and add 益智仁Yizhiren to reduce the common leakage of the elderly with dementia Urinary and incontinence problems.
There are many research that the herbs above helps the Cognitive Function. Will share with you in the laterarticle.
Reference
- Lin SK, Tsai YT, Lo PC, Lai JN. Traditional Chinese medicine therapy decreases the pneumonia risk in patients with dementia. Medicine (Baltimore). 2016 Sep;95(37):e4917. doi: 10.1097/MD.0000000000004917.
- Lin SK, Yeh CH, Lai JN. Demographic and medication characteristics of traditional Chinese medicine users among dementia patients in Taiwan: A nationwide database study. J Ethnopharmacol. 2014 Dec 17. pii: S0378-8741(14)00886-1.
- Lin SK, Yan SH, Lai JN, Tsai TH. Patterns of Chinese medicine use in prescriptions for treating Alzheimer’s disease in Taiwan. Chin Med. 2016 Mar 28;11:12. doi: 10.1186/s13020-016-0086-9.
- http://shunkulin.blogspot.com/2015/08/Chi-Love-Soup.html
- https://herbaltcm.sn.polyu.edu.hk/en/herbal/thinleaf-milkwort-root
-
Review: Acupuncture Treatment for Alzheimer’s Disease

Background: This review aims to systematically summarize and analyze recent high-quality animal research results about the use of acupuncture in Alzheimer’s disease patients. This information will be useful in providing a reference for future experimental research and an experimental basis for the clinical use of acupuncture in the treatment of Alzheimer’s disease
Methods: We utilized and referenced various electronic libraries from their inception to November 2021. Relevant information was reviewed and information such as the journal names, publication records, animal model selections and preparations, intervention measures, acupoint selections, detection methods, and detection indicators was extracted. Results. A total of 75 eligible studies were selected for additional review. Male SAMP8 mice, APP/PS1 double transgenic mice, Sprague-Dawley (SD) rats, and Wistar rats were the four commonly used animal strains in the experiments. The animals were categorized as transgenic and surgical mouse models. Experimental interventions included manual acupuncture (MA), Electro-acupuncture (EA), Moxibustion, and EA combined with Moxibustion.
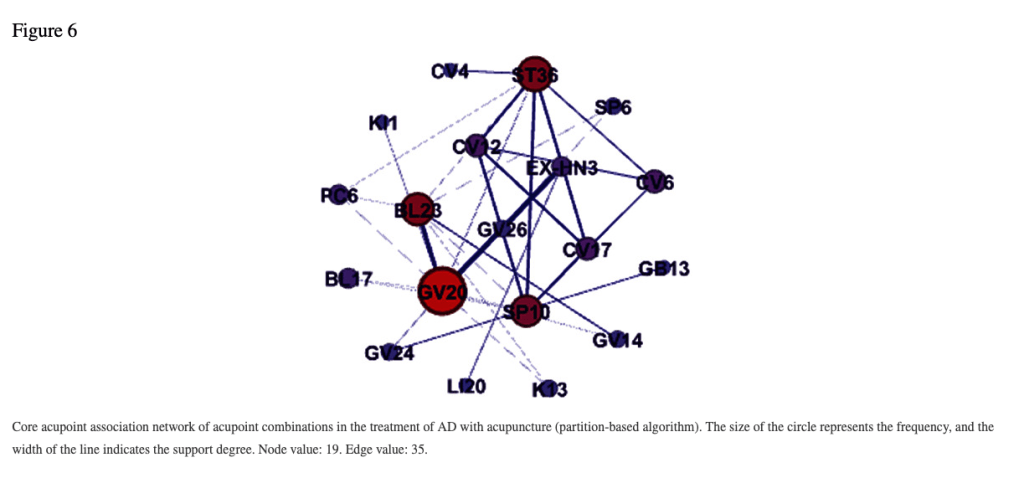
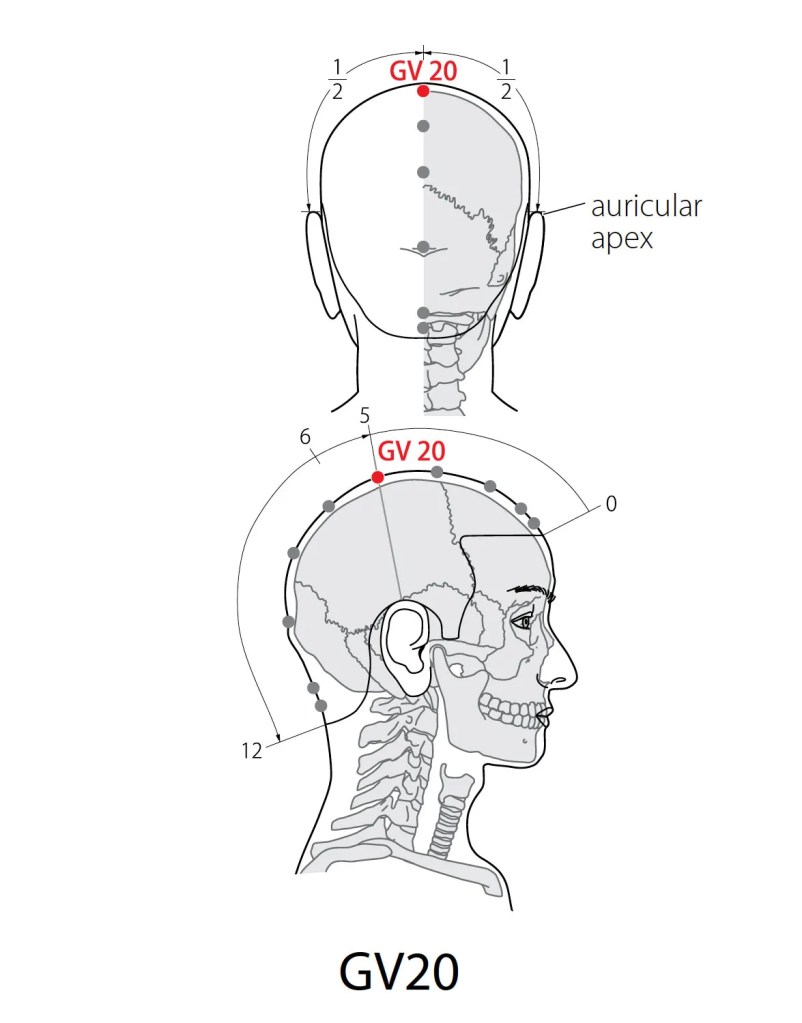
A retention time of 20 min was the optimal timing for experimental studies, with 14 sessions chosen as the most common treatment time. EA was the most prescribed acupuncture treatment type with continuous wave, 2 Hz frequency, and 1 mA electric current selected as frequently used parameters. A total of 78 acupoint prescriptions were analyzed involving 21 acupoints. The top 3 combinations of common acupoints were GV20 ⟶ EX-HN3, GV20 ⟶ BL23, and GV20 ⟶ GV26. A total of 39 articles had positive drug control groups, sham acupuncture, and/or nonacupoint control groups. Furthermore, 10 types of behavioral tests, 29 detection methods, 178 evaluation indicators, and 18 tissue samples were included in the analysis.
Conclusions: By collating these high-quality research studies systematically and comprehensively, acupuncture was found to be a viable and effective treatment in Alzheimer’s disease animal models.
Reference:
Ke C, Shan S, Fang C, Xia Y, Zhang W. A Review on Characteristics of Experimental Research on Acupuncture Treatment for Alzheimer’s Disease: Study Design. Evid Based Complement Alternat Med. 2022 Jul 9;2022:8243704. doi: 10.1155/2022/8243704. PMID: 35855822; PMCID: PMC9288276.
-
Effect of Korean Red Ginseng on Cognitive Function and Quantitative EEG in Patients with Alzheimer’s Disease: A Preliminary Study

Ginseng on Cognitive Function

Background: Korean red ginseng (KRG) has a nootropic effect. This study assessed the efficacy of KRG on cognitive function and quantitative electroencephalography (EEG) in patients with Alzheimer’s disease (AD).
Methods: Fourteen patients with AD (mean age, 74.93 years; 11 women and 3 men) were recruited and treated with KRG (4.5 g per day) for 12 weeks. Cognitive function was assessed by the Korean Mini-Mental State Examination (K-MMSE) and the Frontal Assessment Battery (FAB). EEG performed before and after treatment were analyzed with quantitative spectral analysis.
Results: The FAB score improved significantly after 12 weeks of treatment. In the relative power spectrum analysis performed according to responsiveness, alpha power increased significantly in the right temporal area of the responders. The increments of relative alpha power in the right temporal, parietal, and occipital areas were significantly higher in the responders than the nonresponders.
Conclusions: This study indicates the efficacy of KRG on frontal lobe function in AD, related to increasing relative alpha power.
Reference : https://pubmed.ncbi.nlm.nih.gov/26974484/
-
Subscribe
Subscribed
Already have a WordPress.com account? Log in now.

